Two Pandemics: One Serious, One Mild

Epidemiological modeling has played a central role in the global response to the novel coronavirus (COVID-19) outbreak of early 2020. The response to the emerging pandemic prompted multiple teams of researchers to rapidly adapt existing models, predominantly from previous influenza outbreaks, to forecast the spread of COVID-19 as well as its anticipated fatality rates.
Using the familiar SIR/SEIR epidemiology models, these studies attempt to employ modern statistical techniques to predict the spread and expected mortality of the COVID-19 pandemic. Common approaches include mechanistic adaptations of agent-based simulation to the SIR/SEIR framework that probabilistically estimate the spread of the virus through general social interactions, as well as autoregressive forecasting techniques that update to reflect emerging data for the disease’s spread in a specific country or locale. In both cases, the associated models have been used to strongly advise the adoption of non-pharmaceutical policy interventions as a primary tool of COVID-19 mitigation.
These interventions, consisting of the now-familiar suite of public event cancellations, school and business closures, and wide scale lockdowns or shelter-in-place orders (SIPOs), were implemented in all but a handful of countries across the globe – often with direct dependence on the advice of epidemiology modeling. In a well-documented example, the influential simulation model for the United Kingdom and the United States by researchers at Imperial College London (ICL) spurred both governments to shift their response strategies to embrace wide scale lockdowns in mid-March 2020.
American President Donald Trump and UK Prime Minister Boris Johnson directly credited this model for their respective decisions to impose lockdowns, and Trump continues to cite the ICL projections of up to 2.2 million deaths to justify his actions. These fantastical claims increasingly diverge from the realities of the coronavirus outbreak. In the time since its release back in March, the ICL model has repeatedly failed to accurately anticipate the course of the pandemic in both countries, and in its adaptation to other locales such as Sweden.
While most of the policy discussion has thus far focused on society-wide interventions aimed at reducing the spread of COVID-19 in the general population, the problem of acute outbreaks within long-term care facilities (LTCs) such as nursing homes is now difficult to deny. Although LTC outbreak data vary widely in scope and quality by state and country, a high concentration of COVID-related deaths in such facilities is readily apparent. Depending on jurisdiction, it is not uncommon to find between 30 and 70 percent of recorded COVID-19 fatalities have occurred in nursing homes, including more than half of all recorded deaths in Europe. Similar patterns appear in most US states.
The concentration of outbreaks in LTCs has only recently called attention to a shortcoming of the epidemiological modeling approach that guided the world’s COVID-19 response strategies. While these models aim to project the disease’s spread through social interactions within the general population, they do not appear to be suitable for capturing acute outbreaks among susceptible populations in LTCs and similar closed-residential facilities.
Indeed, we may find this shortcoming directly acknowledged in the 2006 influenza pandemic study that the Imperial College team used as the basis of their COVID-19 simulation. As its authors conceded at the time, “Lack of data prevent us from reliably modelling transmission in the important contexts of residential institutions (for example, care homes, prisons) and health care settings.”
The conundrum presented by LTC outbreaks vis-à-vis epidemiological modeling need not be speculative though, as emerging statistical patterns are beginning to reveal a sharp divergence in the pandemic’s course when trends in such facilities are compared to the general population. Although LTC outbreaks have accounted for significant shares of COVID-19 mortality in all 50 states, obtaining accurate and daily LTC data remains a challenge.
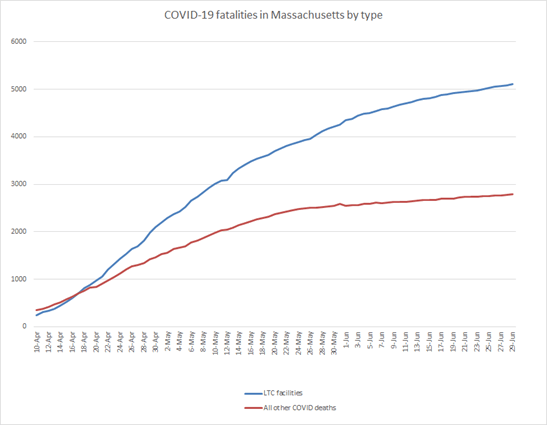
The Commonwealth of Massachusetts presents an exception to this data deficit. Ranking among the hardest-hit of US states outside of the New York City region, Massachusetts began tracking detailed daily COVID-19 case and mortality statistics for LTC facilities on April 10, 2020. At this relatively early stage in the pandemic, LTC and non-LTC fatalities in Massachusetts sat at near-parity. They then began to rapidly diverge. As of June 29, LTC deaths account for 5,111 out of 7,895 confirmed deaths in the commonwealth, or 64.7 percent of all fatalities
The clear patterns in these data suggest that the coronavirus would be better understood if we began to treat it as two simultaneous pandemics: one severe but acute outbreak that ravages nursing homes and LTCs with extremely high fatalities concentrated among the elderly and infirm, and a second significantly milder wave in the general population.
As nearly all mitigation strategies have focused on containing the spread in the general population through lockdowns and similar mandates, the policy response has almost entirely missed the mark despite unleashing unprecedented devastation to our economy and social fabric.
Daily data from Massachusetts illustrate the divergence of the two simultaneous pandemics. As may be seen in the chart below, they show steady growth in the share of COVID-19 deaths arising from LTC facility outbreaks since the beginning of record keeping. Furthermore, these two trends continue to split apart. For the month of June, Massachusetts averaged only 9 COVID-19 deaths per day in the general population. By contrast, the state’s LTC facilities averaged 27 deaths per day despite comprising a tiny share of the population.
When smoothed using a 7-day moving average, daily deaths in the non-LTC general population peaked in late April and began to sharply decline in late May 2020. While Massachusetts LTC deaths have leveled from their early peak around the same time, they still remain at approximately three times the general population’s daily toll.
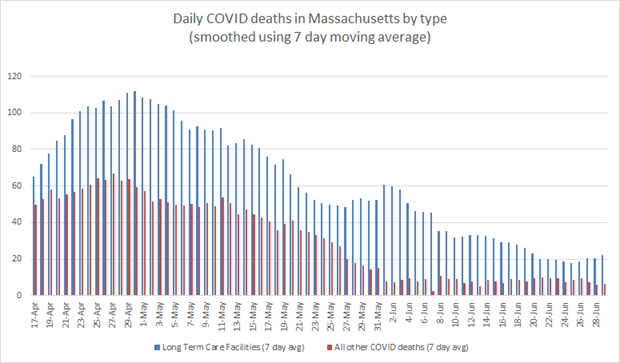
Note: Massachusetts changed its counting methodology on June 1 to include probable COVID-19 deaths that were not confirmed by direct testing. The brief spike in LTC deaths from around this time is likely an artifact of this change in reporting, and not the brief spike observed in the chart
The severity of the LTC outbreak may be seen in the cumulative death toll from this subset of the population. As of this writing, COVID-19 mortalities appear to encompass almost 10 percent of the commonwealth’s pre-pandemic LTC population of an estimated 53,000 residents. By comparison, the state’s approximately 2,784 non-LTC general population deaths as of June 30 come from an estimated 6.9 million people.
The clear difference between observed patterns in LTCs and the general population points to a need to further assess the suitability of current COVID-19 epidemiological modeling strategies in accurately capturing the dynamics of the ongoing pandemic. Indeed, the modeling approach appears to project an entirely different mortality pattern than what we are observing in realized data – even when cumulative death totals approximate some of the milder modeled scenarios from the ICL model and similar projections.
Since most policy interventions aimed at mitigating COVID-19 were premised upon models depicting its general population spread, the emerging evidence of a very different pattern concentrated in LTC facilities is of high consequence in evaluating the political interventions adopted back in March.
Simply put, we adopted the wrong measures and used them to ineffectually target the milder of the two pandemics, all the while neglecting or even exacerbating the much more severe outbreak that continues to run its course through our vulnerable nursing home population.











