Covid Misclassification: What Do the Data Suggest?

According to Worldometer, U.S. deaths from Covid-19 were 272,254 as of 11/29/2020. What are “deaths from Covid-19?” One definition would be deaths where Covid-19 was the primary cause. An example would be a patient who has a positive polymerase chain reaction (PCR) test for the virus responsible for Covid-19 and a clinical picture of hypoxemia, bilateral pulmonary infiltrates on imaging, no obvious other cause, such as influenza or congestive heart failure (CHF), and who dies from progressive acute respiratory distress syndrome (ARDS).
Another definition would be deaths where Covid-19 was a contributing cause but not necessarily the primary disease. An example would be a patient with diabetes or end-stage renal disease who develops an upper respiratory infection URI, has a positive PCR test, never recovers from the URI, deteriorates over many weeks to months and eventually dies.
In this case the underlying cause of death was the diabetes or end-stage renal disease weakening the host defenses and the Covid-19 was the precipitating cause of acute illness and eventual death. Another definition would be a patient who dies, has a positive PCR test, but the Covid-19 clearly had nothing to do with the death. An example would be a trauma victim who had no respiratory symptoms prior to trauma and coincidentally has a positive PCR test.
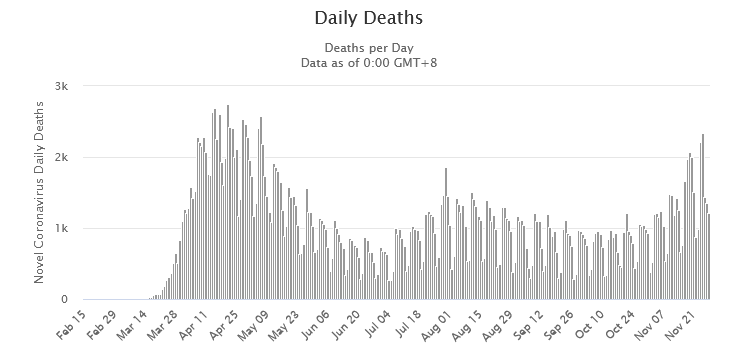
Figure 1: Daily U.S. deaths attributed to Covid-19. Data are from Worldometer as of 11/29/2020.
Figure 1 illustrates the death count from Covid-19. These data are based on death certificates. If the death certificate includes Covid-19, then the death is included whether or not Covid-19 was the primary or even contributing cause of death. The problems with these data are uncertainties about how many deaths are merely associated with Covid-19 rather than caused by Covid-19.
These uncertainties are not helped by the fact that many of these patients are cared for at university medical centers, the death certificates are often filled out by resident physicians in training, and these resident physicians receive no formal training on how to fill out the certificates. These uncertainties are not helped by the fact that the hospital receives a bonus payment for patients who have the ICD-10 diagnostic code for Covid which is included in the problem list for every patient with a positive PCR test. Therefore, a financial incentive exists to perform PCR testing on every patient and label every patient with a positive PCR test as having Covid-19.
One way to sort out these uncertainties is by comparing deaths in 2020 to deaths in previous years. This is sometimes called excess deaths. At least one study has used this methodology to question the narrative about numbers of Covid deaths. This study looked at total deaths from all causes. I will expand on this method by looking at categories of cause of death separately. The Centers for Disease Control (CDC) separates deaths into 5 categories: respiratory diseases, circulatory diseases, malignant neoplasm, Alzheimer disease and dementia, and other select causes.
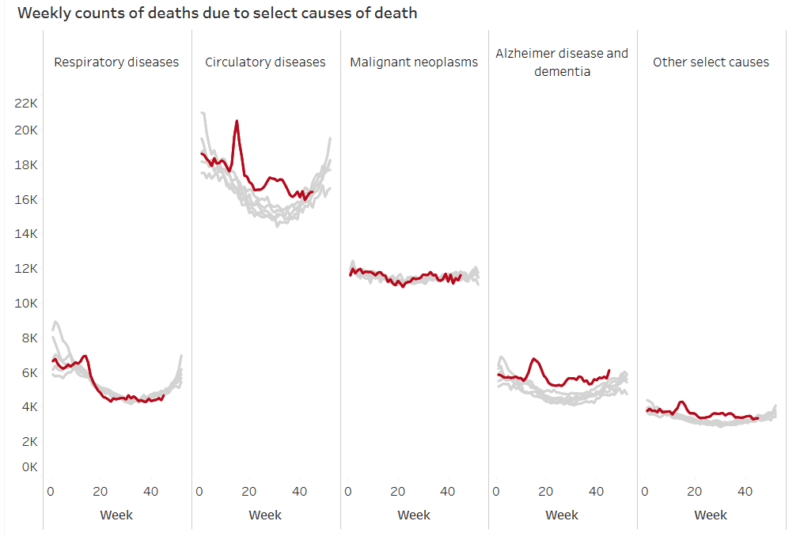
Figure 2: Deaths by week of the year. Data are from the CDC. Gray curves are data for years 2015-2019. Brown curves are for the current year 2020.
Figure 2 illustrates the 5 categories of cause of death. The panel for malignant neoplasms shows that nothing unusual happened in 2020 for this cause of death. The other panels all have a spike occurring between week 15 and 20 which corresponds to the first wave of the Covid pandemic around April and May. These other panels also have similar shapes with a decline from Week 15 to about Week 25, and a second wave peaking between Week 30 and Week 35. The most recent data from around Week 40 should be considered incomplete due to incomplete reporting. Although the curves in these other panels have similar shapes, the level of the current year compared to previous years is much different for the panel illustrating deaths from respiratory diseases.
From about Weeks 18-22, the deaths from respiratory diseases appear to be less in 2020 than in previous years. How can a respiratory illness like Covid-19 have caused fewer respiratory deaths than previous years yet be blamed for the increase in deaths from all causes? The most notable excess in deaths after Week 20 are occurring from circulatory disease. Circulatory disease includes deaths caused by hypertension, stroke, congestive heart failure, and myocardial ischemia.
It is possible that some deaths from circulatory disease should be attributed to Covid-19. An example would be a patient who comes in with Covid-19 respiratory disease, eventually has cardiac arrest after 30 days on a mechanical ventilator, and the resident who fills out the death certificate is only aware of the cardiac arrest and was not involved in the 30 days leading up to the cardiac arrest. The resident may get a notice to fill out the death certificate a week after the incident and does not even remember the case other than being called in the middle of the night for a “Code Blue.”
It is also possible that a clear case of circulatory death is misattributed to Covid-19. An example would be a patient who has an acute myocardial infarction and cardiac arrest, is brought to the hospital by emergency medical services (EMS), has a nasal swab obtained in the emergency department (ED) along with a zillion other lab tests, and dies in the ED. The ED physician filling out the death certificate a week later has been instructed by the hospital employing the ED physician to label every death with a positive PCR test as a Covid death and does so.
How many patients are incorrectly labeled as non-Covid circulatory deaths when they are clearly Covid related? We do not know, but the financial incentives are against this type of error. How many patients are incorrectly labeled as Covid deaths when the positive PCR test result had nothing to do with the cause of death? We do not know, but the financial incentives favor this type of error.
Why would there be an excess of deaths from acute myocardial infarction where Covid was not responsible? The obvious explanation is the lockdown response to Covid-19 made maintenance health care and urgent health care less available. Clinics were largely shut down. Zoom visits were possible for established patients but not for new patients. It is very plausible that excess circulatory deaths were not caused by Covid-19 but rather the authoritarian lockdowns in response to Covid-19.
The above issue of death by lockdown becomes more important when considering the panel for Alzheimer disease and dementia. While Covid-19 could plausibly be the precipitating factor for a circulatory death, it is not plausible that Covid-19 precipitated a case of dementia. There would be little or no reason for resident physicians to mislabel a death caused by Covid-19 as a dementia death.
These deaths are almost certainly due to the lockdown response to Covid-19 which led to reduced maintenance care for patients with dementia who require a lot of maintenance care every day. Even during the April peak, excess deaths from dementia were greater than excess deaths from all respiratory disease. This is very difficult to explain by any hypothesis other than death by lockdown.